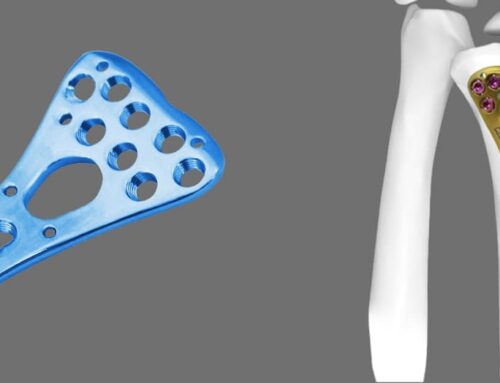
The Locking Medial Distal Tibia Plate is a specialized orthopedic implant used primarily in the surgical treatment of fractures of the distal (lower) third of the tibia. It belongs to a category of implants known as locking compression plates (LCPs) and is commonly used for internal fixation of complex fractures, especially those that are intra-articular, periarticular, or metaphyseal in nature.
Design and Features
Anatomical Contouring:
The plate is pre-contoured to match the anatomy of the medial aspect of the distal tibia. This minimizes the need for intraoperative bending and shaping, reducing surgical time and improving implant fit.
Locking Screw Technology:
The plate features holes for locking screws, which thread into the plate itself, creating a fixed-angle construct. This differs from traditional compression plates, where screws compress the bone to the plate.
Low-Profile Design:
The plate has a low-profile to minimize soft tissue irritation, especially critical in the distal tibia, where soft tissue coverage is minimal.
Combination Holes:
Some holes are designed to accommodate both locking and non-locking screws, offering versatility in fixation.
Multiple Screw Options:
The distal portion of the plate has multiple screw holes at various angles, allowing for subchondral support and multidirectional fixation of the distal fragments, which is crucial in periarticular fractures.
Material:
Typically made of stainless steel or titanium, providing strength, biocompatibility, and resistance to corrosion.
Indications for Use
The Locking Medial Distal Tibia Plate is indicated for:
Distal Tibial Fractures:
- Extra-articular fractures (e.g., AO/OTA 43-A)
- Partial articular fractures (e.g., 43-B)
- Complete articular fractures (e.g., 43-C)
Complex Periarticular Fractures:
Fractures extending into the joint surface that require precise anatomical reduction.
Metaphyseal Fractures:
Fractures near the metaphysis, often seen in osteoporotic bone.
Fractures with Poor Bone Quality:
Locking plates provide better fixation in osteoporotic or comminuted fractures where traditional plating might fail.
Open Fractures:
Often used in staged procedures for open fractures where external fixation is converted to internal fixation once the soft tissues are stable.
Malunions/Nonunions:
Used in corrective surgeries for previous fractures that did not heal properly.
Biomechanical Principles
Angular Stability:
Locking screws create a fixed-angle construct, providing angular stability. This is especially advantageous in osteoporotic or comminuted fractures.
Bridging Technique:
The plate can act as an internal fixator, bridging the fracture site without directly compressing the bone, preserving the periosteal blood supply and promoting biological healing.
Minimally Invasive Plate Osteosynthesis (MIPO):
Often used with minimally invasive techniques to reduce soft tissue damage and promote faster recovery.
Load Sharing:
The construct allows for load-sharing between the bone and the implant, reducing stress shielding and promoting natural bone healing.
Surgical Technique
Preoperative Planning:
- Obtain AP and lateral radiographs or CT scans for complex fractures.
- Choose appropriate plate length based on fracture pattern and bone size.
Patient Positioning:
- Typically, supine on a radiolucent table for intraoperative imaging.
Approach:
- A medial approach to the distal tibia is common.
- In minimally invasive techniques, small incisions are made proximally and distally.
Fracture Reduction:
- Achieve anatomical reduction of the articular surface.
- Use temporary fixation (K-wires, clamps) before plate application.
Plate Application:
- Position the plate on the medial aspect of the tibia.
- Confirm position with fluoroscopy.
- Insert distal locking screws first to secure the articular fragments.
Proximal Fixation:
- Insert non-locking screws first to compress the plate to the bone, if needed.
- Follow with locking screws to complete the fixation.
Final Checks:
- Confirm reduction and hardware placement with imaging.
- Close soft tissues in layers.
Postoperative Care
Weight-Bearing:
- Typically non-weight-bearing initially.
- Progress to partial weight-bearing and then full weight-bearing based on healing, usually guided by follow-up imaging.
Rehabilitation:
- Early range of motion exercises for the ankle joint to prevent stiffness.
- Strengthening and proprioception exercises once healing progresses.
Follow-up:
- Regular radiographic evaluation to monitor healing and detect complications.
Complications
Infection:
- Especially in cases of open fractures or compromised soft tissue.
Nonunion/Delayed Union:
- Can occur if biological healing is compromised.
Malalignment:
- Risk of varus/valgus malalignment if reduction isn’t precise.
Hardware Irritation:
- The medial aspect of the tibia has minimal soft tissue coverage, which can lead to hardware prominence or irritation.
Screw Loosening/Breakage:
- Less common with locking plates but can occur in poor bone quality.
Stiffness:
- Especially at the ankle joint if early mobilization is delayed.
Advantages over Traditional Plates
Enhanced Stability:
Locking screws provide greater stability, particularly in osteoporotic or multifragmentary fractures.
Reduced Need for Precise Plate-Bone Contact:
The fixed-angle nature of locking plates reduces the reliance on plate-bone compression, preserving periosteal blood supply.
Minimized Soft Tissue Damage:
Compatible with MIPO techniques, leading to faster recovery and fewer soft tissue complications.
Versatility:
Combination holes allow for both locking and non-locking screws, adapting to different fracture patterns.
Conclusion
The Locking Medial Distal Tibia Plate represents a significant advancement in orthopedic trauma surgery, offering improved outcomes for challenging distal tibial fractures. Its anatomical design, locking technology, and compatibility with minimally invasive techniques make it a preferred choice for surgeons dealing with complex fracture patterns, particularly in cases involving poor bone quality or soft tissue concerns. Proper surgical technique, combined with appropriate patient selection and postoperative management, is key to achieving optimal results.



Leave A Comment